- Daily Industry Report
- Posts
- Daily Industry Report - October 28
Daily Industry Report - October 28

Your summary of the Voluntary and Healthcare Industry’s most relevant and breaking news; brought to you by the Health & Voluntary Benefits Association®
Jake Velie, CPT | Robert S. Shestack, CCSS, CVBS, CFF |

By HVBA - The Health & Voluntary Benefits Association (HVBA), in partnership with the Workplace Benefits Association (WBA), is honored to announce the induction of David Essary, Chief Strategy Officer at Alight Solutions, into the prestigious HVBA & Workplace Benefits Association International Hall of Fame. This distinguished recognition celebrates David’s exceptional leadership, strategic vision, and lasting contributions to the voluntary benefits and healthcare landscape. Read Full Article...
HVBA Article Summary
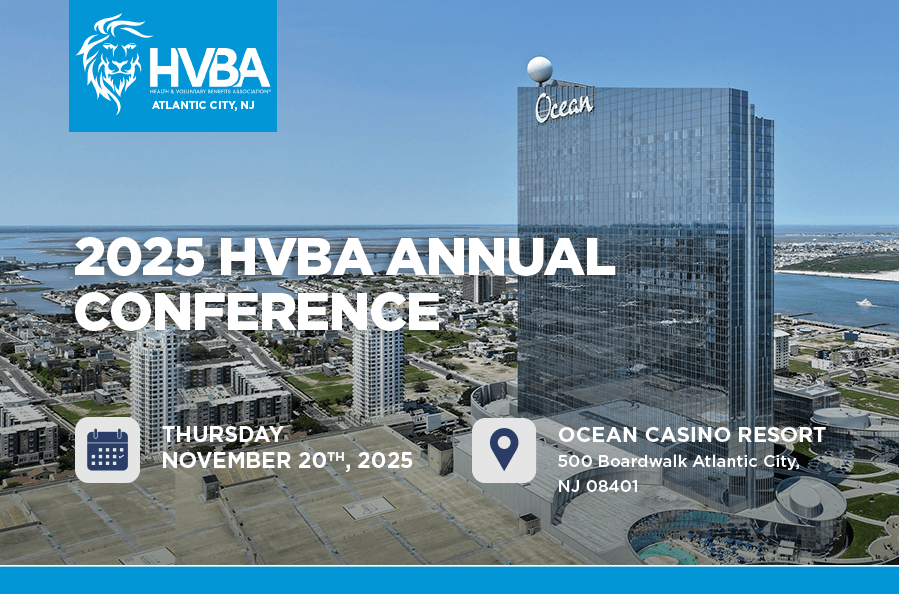
David Essary to Be Inducted into HVBA Hall of Fame: David Essary will receive a prestigious honor at the 18th Annual HVBA Conference, set for Thursday, November 20, 2025, at the Ocean Casino Resort in Atlantic City, NJ. As one of nine distinguished honorees, Essary is being recognized for his exceptional leadership and long-standing contributions that have significantly shaped the voluntary benefits industry on a national scale.
Recognition of Industry Leadership and Innovation: Known for his deep strategic insight and ability to communicate complex benefits concepts, Essary’s career—most notably at Allstate—has helped transform how employers support their workforce. His Hall of Fame induction reflects decades of trailblazing work in benefits modernization, employee education, and expanding access to meaningful healthcare and financial wellness solutions.
Event Sponsored by Humana, Open for Industry Participation: Sponsored by Humana, the HVBA’s 18th Annual Conference will not only feature the Hall of Fame ceremony but also present eight Leadership Awards, celebrating individuals who continue to drive excellence in the sector. The event is positioned as a key gathering for professionals across the voluntary benefits and healthcare space, with registration now open and strong early demand for attendance and sponsorship opportunities.
HVBA Poll Question - Please share your insightsLooking ahead to 2026, select the grouping that best reflects your business/customer priorities, from High Priority (1) to Low Priority (4): |
|
Our last poll results are in!
39.29%
Of the Daily Industry Report readers who participated in our last polling question reported they “Strongly support” the U.S. policy to impose a 100% tariff on imported branded/patented drugs unless companies build production locally, and that “it will encourage domestic drug manufacturing.”
26.19% of respondents ”Somewhat support” the tariff policy “with safeguards to protect consumers.” On the contrary, 17.26% “Somewhat oppose” responding that “it risks increasing drug prices and supply issues,” while the remaining 17.26% “Strongly oppose,” and believe “it’s bad policy that will harm patients and innovation.”
Have a poll question you’d like to suggest? Let us know!
Cigna Evernorth unveils rebate-free pharmacy model cuts costs, simplifies pricing
By Ella Jeffries – The Cigna Group’s Evernorth division introduced a rebate-free pharmacy benefit model that it says will lower medication costs and simplify drug pricing. The model removes the traditional post-purchase rebate structure by applying negotiated drug discounts upfront, according to an Oct. 27 news release. Patients will pay the lowest available cost — whether it’s Evernorth’s negotiated rate, a copay, cash price or a direct-to-consumer offer. For example, if a medication is priced at $22 under Evernorth’s discount, but has a $20 cash price, patients would pay $20. Read Full Article...
HVBA Article Summary
Rebate-Free Model Aims to Lower Costs: Evernorth's new pharmacy benefit model eliminates the traditional rebate system, instead offering upfront discounts on medications. This approach is designed to ensure patients always pay the lowest available price, regardless of whether it is a negotiated rate, copay, or cash price. The model is intended to make drug pricing more transparent and predictable for consumers.
Implementation Timeline and Scope: The model will be rolled out to fully insured Cigna members in 2027 and will become the standard for all Evernorth pharmacy benefit clients by 2028. Evernorth's pricing tool, which already serves tens of millions of Americans, is expected to expand further in January 2026. This phased implementation suggests a broad impact across the company's client base over the next few years.
Additional Changes for Pharmacies: Alongside the new pricing model, Evernorth will update its reimbursement structure for in-network pharmacies in 2026. The revised system will cover medication costs, dispensing fees, and introduce performance-based clinical incentives. These changes are likely aimed at aligning pharmacy incentives with patient outcomes and supporting the transition to the new benefit model.
John Oliver Takes on Medicare Advantage
By Wendell Potter – Last night’s episode of Last Week Tonight with John Oliver turned its spotlight on the troubling world of Medicare Advantage — the privately-run alternative to traditional Medicare that HEALTH CARE un-covered and others have long questioned in terms of cost, fairness and value. Most folks don’t even know what Medicare Advantage is, let alone how deeply flawed the program has become and how much it drains the Medicare Trust Fund. But most people have seen the ads on TV – which Oliver suggests shouldn’t even be allowed to have the word “Medicare” included because that in itself is deceptive (and several lawmakers agree with him). Read Full Article...
HVBA Article Summary
Medicare Advantage's Financial Impact: Independent analyses have shown that Medicare Advantage costs taxpayers significantly more than traditional Medicare. This increased spending is attributed to the way these private plans are structured and reimbursed. The financial burden on the Medicare Trust Fund raises concerns about the program's long-term sustainability and the value it provides to both seniors and taxpayers.
Barriers to Care for Seniors: Seniors enrolled in Medicare Advantage plans often encounter narrower provider networks and more frequent prior-authorization requirements compared to traditional Medicare. These restrictions can result in delays or denials of necessary medical care, disproportionately affecting older adults and people with disabilities who may already face health and financial vulnerabilities. The article highlights that these features mirror some of the most criticized aspects of private insurance.
Calls for Reform and Industry Resistance: There is growing bipartisan interest in reforming the Medicare Advantage program due to concerns about deceptive advertising and burdensome practices. Despite this momentum, the insurance industry is expected to spend heavily on lobbying efforts to protect its profits from the program. The article suggests that without significant policy changes, many seniors will continue to be affected by the shortcomings of Medicare Advantage.
Why GLP-1 coverage alone isn't enough
By Ray Fabius, M.D., FAAP, FACPE – As the obesity epidemic accelerates, employers are facing mounting pressure to address weight management in their benefit strategies. The World Health Organization predicts that overweight and obese populations worldwide will reach $3 trillion per year in U.S. dollars by 2030 and more than $18 trillion by 2060. GLP-1 medications, such as Semaglutide and Tirzepatide, have emerged as powerful tools that deliver significant weight loss and also reduce the risk of diabetes and cardiovascular disease. But as brokers and consultants know, these drugs come with a steep price tag and the real value to employers and employees depends on more than just coverage. Read Full Article... (Subscription required)
HVBA Article Summary
GLP-1 Medications Are Effective but Costly: GLP-1 drugs have demonstrated significant clinical benefits, including sustained weight loss and reduced risk of diabetes and cardiovascular events. However, their high cost has led to increased pharmacy spending for employers who offer coverage. This financial impact makes it essential for organizations to consider the broader value and sustainability of simply covering these medications.
Comprehensive Programs Enhance Outcomes: Evidence suggests that GLP-1 medications are most effective when combined with lifestyle interventions such as nutrition and physical activity programs. Patients who discontinue the drugs often regain weight unless they maintain healthy habits, highlighting the importance of integrated support. International practices reinforce this approach by requiring nutritional counseling and specialist oversight alongside medication.
Strategic Benefit Design Is Needed: Employers are encouraged to adopt a value-driven approach that integrates GLP-1 coverage within a holistic weight management program. This includes mandatory participation in lifestyle programs, access to behavioral health resources, and step therapy with less expensive medications when appropriate. Such comprehensive strategies not only improve health outcomes but also help justify the investment in high-cost treatments.
12 states with the highest uninsured rates
By Allison Bell – The U.S. federal government is now considering proposals for health insurance subsidy rules that could lead to a big increase in the number of people who lack either public or private health coverage. A big increase in the uninsured rate could hurt employer-sponsored health plans in many ways. Doctors and hospitals may try to shift the cost of treating uninsured patients onto the backs of employers, and providers in communities with many uninsured patients may start to deliver lower-quality, less convenient care. Read Full Article... (Subscription required)
HVBA Article Summary
Potential Increase in Uninsured Population: The federal government is reviewing health insurance subsidy proposals that might significantly raise the number of uninsured individuals. This potential rise could reverse recent improvements in coverage rates and increase the financial burden on healthcare providers and employers. Such changes may also impact the stability and cost structure of employer-sponsored health plans.
Impact on Healthcare Providers and Employers: Higher uninsured rates can lead doctors and hospitals to shift the costs of uncompensated care to employers, potentially increasing employer healthcare expenses. Additionally, communities with many uninsured residents might experience a decline in the quality and accessibility of healthcare services, affecting overall public health outcomes. This dynamic could strain employer-sponsored insurance systems and healthcare delivery.
Recent Trends in Uninsured Rates: According to the American Community Survey, the median uninsured rate in U.S. states decreased from 8% in 2019 to 7.1% in 2024. Despite this improvement, certain states still have high uninsured rates that could negatively affect employer health plans. Understanding these state-level disparities is important for policymakers and employers aiming to address coverage gaps.
What new advertising rules may mean for pharma companies
By Maia Anderson and Kristina Monllos – Seasoned TV watchers are probably accustomed to the ebb and flow of pharmaceutical ads, when depictions of relief are followed by a reminder to talk to a doctor about a particular drug, which then leads into a speedy rundown of the potential side effects of said drug. Those ads, let alone how pharma companies advertise altogether, could soon be changing. President Donald Trump on Sept. 9 signed a memorandum to the Department of Health and Human Services (HHS) and the head of the FDA that would get rid of the 1997 “adequate provision” loophole, which lets prescription drugmakers summarize safety and risk information in TV ads and direct consumers elsewhere to get additional information. Read Full Article...
HVBA Article Summary
Impact on Pharmaceutical Advertising Costs and Strategies: The removal of the 'adequate provision' loophole is expected to make TV advertising for pharmaceutical companies more expensive and complicated. Drugmakers may need to purchase longer and more costly ad spots to include comprehensive safety and side effect disclosures, potentially limiting creative messaging and reducing overall advertising spend. This could lead to a shift where only the largest pharma companies can afford TV advertising, while others might redirect budgets to healthcare professional advertising or unbranded campaigns focusing on conditions rather than specific drugs.
Regulatory Enforcement and Industry Response: The FDA has initiated a crackdown by sending thousands of warning letters and cease-and-desist orders to companies with allegedly deceptive ads across multiple channels, including TV, websites, newsletters, and social media. While the agency has not detailed further enforcement actions, pharmaceutical companies generally comply quickly due to their reliance on FDA approval. Industry representatives express concern that the new rules could hinder patient access to important drug information and complicate advertising efforts.
Challenges with Telehealth and Compounded Drugs Advertising: Telehealth companies promoting compounded drugs, which are not FDA-approved and thus not subject to the same disclosure requirements, present a regulatory challenge. Recent legislative efforts aim to extend FDA oversight to telehealth and influencer drug promotions, but no concrete actions have been taken yet. The ambiguity around regulation in this area adds complexity to the evolving pharmaceutical advertising landscape.
Why activating transparency data is the key to cost containment and member value
By Ben Callaghan – For years, Transparency in Coverage (TiC) has hovered in the background of health plan conversations—a regulatory obligation with little practical impact. Mandated machine-readable files were published, buried on websites, and promptly forgotten. Employers barely noticed. Members never used them. And TPAs, squeezed by compliance deadlines, treated it as just another box to check. Read Full Article... (Subscription required)
HVBA Article Summary
Shift from Compliance to Activation: The article emphasizes that simply meeting regulatory requirements for transparency in health coverage is no longer sufficient. True value comes from actively using transparency data to inform and empower members at the point of care decisions. This shift can transform transparency from a passive obligation into a proactive tool for cost containment and improved member experience.
Role of AI and Technology in Member Engagement: Artificial intelligence and integrated digital tools are highlighted as key enablers for making transparency data accessible and actionable. By delivering real-time, personalized information, these technologies can help members make informed choices without needing to navigate complex plan documents or medical codes. This approach not only streamlines the decision-making process but also increases the likelihood of members engaging with cost-saving opportunities.
Competitive Advantage for TPAs and Employers: Third-party administrators (TPAs) and employers who leverage transparency data to design smarter benefit plans and incentives can gain a significant edge. By rewarding members for cost-effective choices and making savings opportunities visible, organizations can reduce overall health plan costs and enhance member satisfaction. Those who move beyond compliance and fully activate their transparency resources are better positioned to meet rising expectations from both regulators and plan participants.

'An epidemic that keeps growing': Supporting employees through substance use
By Paola Peralta – A substance use disorder isn't just a personal struggle — it's a workplace crisis that requires leaders' immediate attention and intervention. In today's workplace, nearly two-thirds of people suffer from a substance use disorder, according to data from the Center for Diseases Control and Prevention. For organizations, this means that using benefits and policies to address these disorders has become a critical issue for both their business and the health and safety of their employees. "Substance use disorder is an epidemic that keeps growing," says Zakia Natour, the director of people and talent at addiction and recovery platform Eleanor Health. "Access to treatment and reducing the stigma around getting support has come so far, but there's a huge opportunity to continue." Read Full Article... (Subscription required)
HVBA Article Summary
Workplace Impact and Employer Responsibility: Substance use disorders are not only personal health issues but also significant workplace challenges that can affect productivity, safety, and employee well-being. Employers are increasingly expected to address these challenges through targeted benefits and supportive policies. Recognizing substance use as a workplace issue helps organizations take proactive steps to support affected employees and mitigate broader business risks.
Evolving Employer Strategies: Many organizations have expanded their support for employees struggling with substance use by enhancing health plans, introducing telehealth options, and offering specialized employee assistance programs. These efforts reflect a growing understanding that mental health and substance use are interconnected and require holistic solutions. However, experts emphasize that more targeted, transparent, and empathetic approaches are needed to create lasting change and reduce stigma.
Importance of Education and Empathy: Creating a supportive environment for employees with substance use disorders involves ongoing education for both leaders and staff. Open dialogue, empathetic leadership, and safe spaces for discussion can encourage employees to seek help without fear of judgment or reprisal. By prioritizing education and empathy, organizations can foster a culture where employees feel supported in addressing their challenges and achieving their full potential.